NATIONAL GUIDELINES FOR PROLONGED BLEEDING MANAGEMENT
Original Authors on behalf of the ATP: Griffiths M, Oakley S, Hall N, Ganesan K (2020)
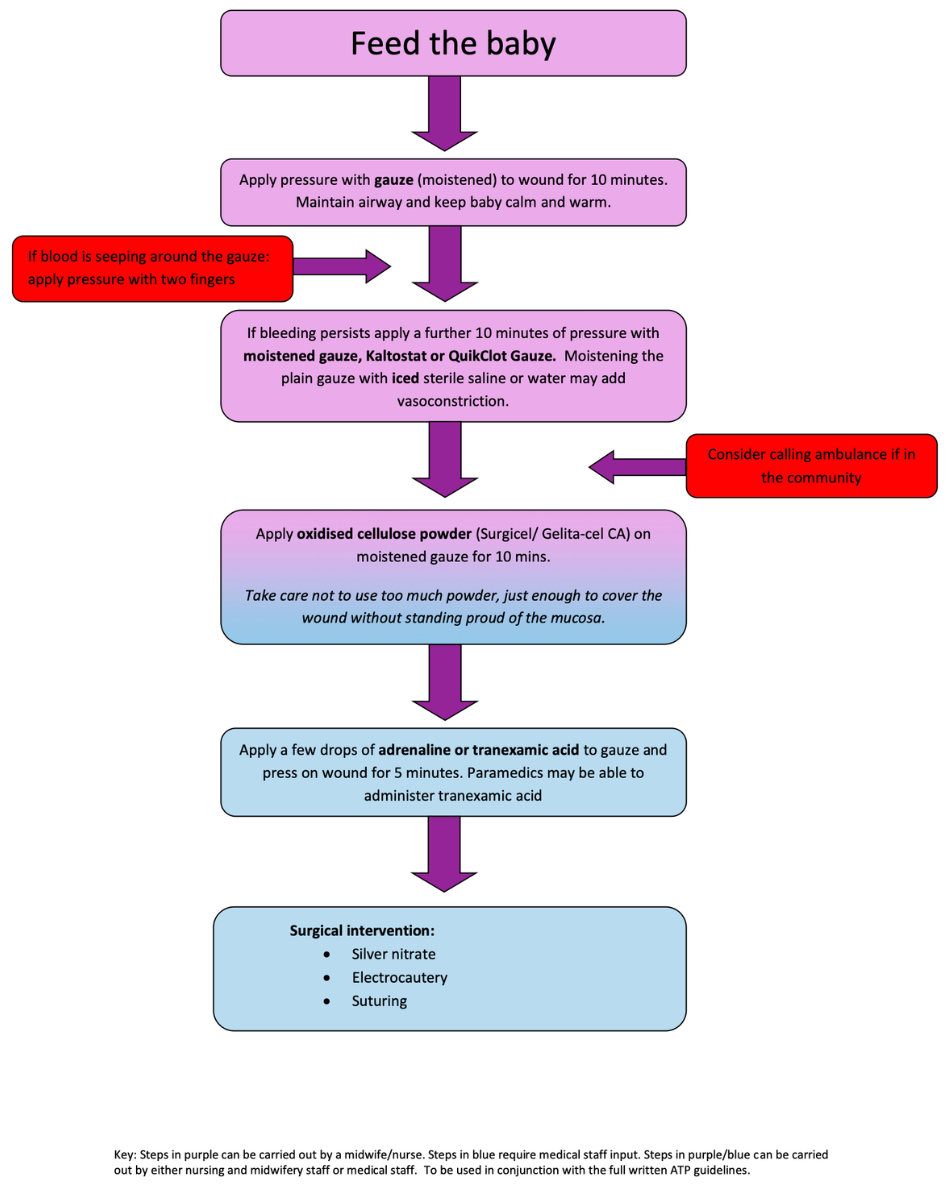
Management of prolonged bleeding post tongue-tie division flow chart 2025
Guideline for the management of bleeding post frenulotomy
This guideline was originally developed by Mervyn Griffiths, Consultant Paediatric Surgeon (now retired), Wessex Tongue-tie Service, Southampton Hospital and Sarah Oakley, Independent Nurse, Lactation Consultant and Tongue-tie Practitioner, Cambridgeshire in 2015. On 23 November 2019 the ATP held a study day looking at the management of bleeding and these guidelines were reviewed by the delegates attending and this document is the result. We are very grateful for the expert advice we have received from Kandy Ganesan, Oral Surgeon, Southend Hospital in updating this guideline and from Nigel Hall (Consultant Paediatric and Neonatal Surgeon, Southampton Children’s Hospital) who reviewed it. An addition to these guidelines was made in early 2024 to include the use of iced sterile water/saline. The use of Quik Clot was added in late 2025. Please read the ‘notes about this guideline’ section for more information.
Incidence of excessive bleeding
A small amount of bleeding post division is common and to be expected. Allowing the baby to feed on the breast or bottle treats this best, as feeding will compress the floor of the mouth. It also clams the baby which will reduce blood pressure and therefore reduce bleeding. A small audit involving 50 practitioners conducted by the ATP in 2018 found that around one in 400 babies will require pressure to settle the bleeding, around one in 7000 will require the application of adrenaline and around one in 77,000 will require cautery or suturing.
Consent
In view of the possibility of a prolonged or heavy bleeding post division, practitioners should take care to ensure this is included in the consent process. Talking through the various steps within this guideline, with parents or guardians, prior to division can be a good way to prepare them and reduce anxiety should a bleed occur.
Risk reduction
Bleeding disorders
Prior to division ask parents/guardians about any family history of haemophilia, Von Willebrand’s, platelet deficiencies and other bleeding disorder or tendency to bleed and document this. Things to consider are:
• Is there a possibility of consanguineous marriage? (E.g. Some Asian families)
• Is the family Jewish? (High incidence of FXI deficiency in Ashkenazi Jews – 8% of the population)
• Are there any signs of easy bleeding/bruising (e.g. site of IM vitamin K injection, Guthrie test, cephalohematoma, bleeding from umbilicus)
If in doubt don’t divide but seek further advice from the family GP, the haemophilia centre for your area, or the medical team looking after the family member affected by the bleeding disorder.
Vitamin K Deficiency Bleeding (VKDB)
The risk of VKDB is low. There are 3 types of VKDB. Early onset occurs within the first 24 hours of life in babies whose mothers are taking certain drugs, including anticonvulsants, anticoagulants and antibiotics. This cannot be prevented by the administration of vitamin K. Classic onset VKDB occurs between days 2-7 after birth. Late onset VKDB is said to occur from 8 days up to 3 months (although there have been cases reported in babies up to 6 months). Vitamin K prophylaxis at birth aims to prevent classic and late onset VKDB. The average incidence of late onset VKDB in high income countries such as the UK is 1 in about 11,000 (WHO cited by Wickham, 2017).
Due to the potential for increased bleeding in babies who have not had vitamin K prophylaxis many NHS Trusts and some private practitioners have policies in place which require that the baby is given vitamin K prior to division or that a clotting screen is done. An alternative approach is to discuss the potential risk factors with parents and document this as part of informed consent. Exclusively breastfed babies (particularly those that are not feeding well) who have not received vitamin K are at increased risk compared to babies who have not received vitamin K and are combination fed or formula fed as formula contains vitamin K. It is for practitioners and services to decide how they will manage this situation. However, all parents/guardians should be asked about vitamin K prophylaxis prior to division and the potential increased risk of bleeding should be considered.
Management of excessive bleeding
If there is an unusual amount of bleeding after division, it is likely to be dark venous bleeding. Bright red arterial bleeding is very rare.
- Hold baby in an upright position. Put some gauze on the raw diamond wound under the tongue and hold in place firmly with one finger, taking care not to place any pressure under baby’s chin as this can obstruct the airway. Moistening the gauze with sterile water, sterile normal saline, cooled boiled water, or breastmilk will help prevent the clot sticking to the gauze and being removed when the gauze is removed. Continue to press for at least 10 timed minutes. Ensure that the airway is maintained. Keep baby warm and calm. Walking round whilst carrying baby, rocking, white noise, music, fresh air, toys, etc can be used to distract and help calm baby.
- The use of iced sterile water or saline at this initial stage has been found in some cases to effectively stem the bleeding. Plastic vials of sterile water or saline for injection or irrigation can be frozen and then thawed slightly by running briefly under warm water. The resulting icy water or saline can then be squirted from the vial onto the gauze which is them immediately applied to the wound.
- If the gauze becomes soaked while you are pressing, you are not pressing in the right place. Replace the gauze and check you are pressing under the tongue on the raw diamond, but now press with two fingers, side by side, to ensure you are pressing on the outer edges as well as the centre. Continue pressure for at least 10 timed minutes.
- Do not continually remove the gauze to see if the bleeding has stopped – wait for at least 10 minutes and then look.
- If bleeding persists apply pressure for a further 10 minutes using gauze or Kaltostat (alginate dressing)* or QuikClot (Kaolin based dressing)**
- If you are not in a hospital, consider calling an ambulance if initial control of the bleeding is impossible or if the bleeding recurs despite successful pressure control.
- This decision should be based on professional judgement and experience considering the level of blood loss, the age, size and condition of the baby and distance to the nearest Accident and Emergency Department. It is never going to be easy, but everyone will err on the side of safety.
- When assessing blood loss consider how much blood baby may potentially swallow during feeding as this may be significant in prolonged bleeding.
- When calling 999 tell ambulance control that you are a healthcare professional seeking assistance with an emergency and when they ask if baby’s breathing is normal say ‘no, it is abnormal’ as oral bleeding and pressure in the mouth will impact breathing and this will mean your call is prioritised for an immediate response.***
- Paramedics may be able to prescribe and administer Tranexamic Acid so this is an option to try prior to transfer to hospital depending on the baby’s condition. ****
- Take any used swabs into hospital with you for estimation of blood loss.
- Take the red book and request the ambulance phone ahead so the relevant team is available on arrival.
- Take a copy of this guideline in too as bleeding post division is rare and A&E departments may not have dealt with it before.
- Document time of division, time of 999 call, time of ambulance arrival, time of arrival in hospital and document names of medical staff who treat baby in hospital.
6. If bleeding persists an oxidised cellulose powder haemostat may be used such as Surgicel Powder Absorbable Haemostat or Gelita-cel CA Powder *** (where practitioners have access to these products and have competency in their use). Place a small amount of powder onto moistened gauze and press onto the wound for 10 minutes. Take care not to use huge amounts of powder as this will displace out of the wound. Essentially you need enough to cover the width of the wound and it shouldn't stand proud above the surface of the mucosa.
7.In a controlled, hospital environment, with suitable monitoring, put a few drops of Adrenaline (1:1000, 1:10000 and 1:100000, or lignocaine 1% with 1:100,000 Adrenaline have all been used) on a gauze swab and press for 5 minutes on to the wound. There is no correct dose, but the potential side-effects of systemic absorption need to be considered when choosing the dose to use.
8. Rebound bleeding is a risk with adrenaline so Tranexamic Acid can be used as an alternative or after the application of Adrenaline. Soak gauze in Tranexamic Acid and apply for 5 minutes.
9. If all this fails, you will have to invoke surgical help… Silver Nitrate, electrocautery and suturing are options at this point.
This group of babies have had a long period of sublingual pressure followed by some form of surgery. This causes considerable oedema and some oral aversion, so they need to be kept under very close supervision, potentially as an inpatient for several days, until they are feeding normally. A prompt naso-gastric tube for initial stress-free feeds is very useful and avoids an unnecessary IV line.
*Kaltostat 10cm x 10cm may be easier to use than 5cm x 5cm and can be cut to make it smaller if needed. It can be obtained through the usual NHS supply chains for dressings or for private practice purchased from Amazon or online medical suppliers.
**QuikClot (10cm x 10cm) can be purchased here QuikClot EMS Haemostatic Gauze Dressing (10cm x 10cm) – TacTree
***This advice on what to say when calling for an ambulance is based on advice given to Sarah Oakley by the East of England Ambulance Service on 22/2/2020.
**** Gelita-Cel CA Powder can be purchased from https://www.deltasurgical.co.uk/ or through normal NHS supply chains.
Reporting
Individual NHS Trusts will have their own systems for reporting instances of bleeding which NHS staff should familiarise themselves with. The same will apply to those working for private companies, hospitals or clinics under ‘practicing privileges’ and other arrangements.
For those working in a self- employed capacity with their own CQC registration we have been advised by the CQC that you should notify them of any bleed where an ambulance is called. You can do this via the CQC notification system or discuss with your own inspector.
The ATP has a voluntary reporting system for all adverse events and we strongly urge all members to participate in this. Your report will be confidential, unless there is a concern about safety. Anonymised data from your report will be used to collate information on how often bleeds occur, which babies are more affected, management strategies, and so on to help advance and inform practice.
Guidance on bleeding for parents
There have been a few reported cases of prolonged and/or heavy bleeding which has occurred sometime after the procedure when the babies have returned home. So, it would seem prudent to provide parents with advice on how to manage this in the very unlikely event it should occur. Below is an example of the kind of guidance you may choose to give to your clients:
There have been reported cases of bleeding which has occurred sometime after tongue-tie division, usually on the same day, when the babies have returned home. If this occurs the bleeding is usually very light and is triggered by strenuous crying (resulting in the tongue lifting and disturbing the wound) or when the wound is disturbed during feeding, particularly if the wound is caught by a bottle teat or tip of a nipple shield.
1. If you notice any blood in your baby’s mouth then offer the baby the breast or bottle and feed them. This will usually stop the bleeding within a few minutes just as it did immediately after the procedure. If the baby refuses to feed then sucking on a dummy/pacifier or your clean finger will have a similar effect.
2. If the bleeding is very heavy or does not reduce with feeding and stop within 15 minutes, then apply pressure to the wound under the tongue with one finger using a clean piece of gauze or muslin for 10 minutes. Do not apply pressure under the baby’s chin as this can affect breathing.
3. If bleeding continues after this time continue to apply pressure to the wound and take your baby to hospital (call an ambulance if you live more than a very short distance from the Accident and Emergency Department).
Advice for parents on managing bleeding is included in the ATP Aftercare Advice Sheets available to order from this website www.tongue-tie.org.uk/shop
IMPORTANT: Notes about this guideline
This document is a guideline only to assist NHS Trusts and private practitioners in developing their own policies and practice in managing bleeding. It is the responsibility of NHS Trusts and private practitioners to ensure that any policies or practices they implement meet the needs of their individual services and situations and any actions included within those policies fall within the competencies of practitioners. Practitioners are accountable for all clinical decisions made in relation to the management of bleeding post division.
Specific research on interventions to manage bleeding in infants post tongue-tie division is not available but papers relating to the use of some of the interventions mentioned within these guidelines in dental and ENT procedures are included in the bibliography.
Heavy and prolonged bleeds are rare so the guidance here is based on strategies used by members of ATP that have been found to be effective. It is up to individual NHS Trusts to develop their own policies on this.
Some NHS Trusts are concerned about using Kaltostat as there is potential for fibres to be left in the wound once the dressing is removed and it is not licensed for use in babies under one year. Other Trusts have taken the view that if it effectively stops bleeding and avoids an escalation to more invasive treatment (such as suturing) which can then prevent a baby feeding orally for several days, then it is a good option. It has been used with varying degrees of success by many ATP members and seems to perform best for moderate bleeding.
The ATP has received an incident report relating to just one case where Gelita-Cel Standard was used and became friable when practitioners tried to remove it. The manufacturer of this product recommends that it is left in situ to be absorbed. However, there are concerns about its adherence (Lui, 2019) and the potential for the dressing to come away and pose a choking risk. For this reason, these guidelines suggest the sparing use of Gelita-Cel CA Powder and this would be left in situ and not removed.
The use of QuikClot has been added to these guidelines in December 2025 after an ATP member witnessed it’s successful use in a baby with post frenulotomy bleeding in an A&E department. The manufacturer was contacted by Sarah Oakley who confirmed it can be used in the oral cavity. They also confirmed that the gauze product was changed in 2008 from a zeolite formula to a kaolin based formula. So there is no risk of exothermic reactions. The correspondence with the manufacturer can be found in Appendix 1.
Bibliography
Ker K, et al (2013) Topical application of tranexamic acid for the reduction of bleeding. Cochrane Systematic Review.
Lui L, et al (2019) Topical biomaterials to prevent post-tonsillectomy haemorrhage. Journal of Otolaryngology-Head & Neck Surgery. 2019 48:45
Huang L, et al (2020) Advances in Topical Hemostatic Agent Therapies: A Comprehensive Update. Advances in Therapy. Volume 37, pages 4132-4148.
Matthew LR, et al (1994) Alginate fiber dressing for oral mucosal wounds. Oral Surgery, Oral Medicine, Oral Pathology Vol 77, Issue 5, p 456-460
Matthew LR, et al (1993) Tissue response to a haemostatic alginate wound dressing in tooth extraction sockets. British Journal of Oral and Maxillofacial Surgery. Vol 31, Issue 3, p 165-169
Mohareb AM, et al (2018) Effect of topical and systemic tranexamic acid on bleeding and quality of the surgical field during ear exploration surgery: a double-blinded, randomised clinical trial. Journal of Current Medical Research and Practice. Vol 3, Issue 2, p75-80.
Teppo H, et al (2006) Topical adrenaline in the control of intraoperative bleeding adenoidectomy: a randomised controlled trial. Clinical Otolaryngology. Vol 31, Issue 4
Wickham S (2017) Vitamin K and the Newborn.
Appendix 1
On 8 Sep 2025, at 11:37, <***********@teleflex.com> wrote:
Good Morning *****,
Thank you for your patience with this question.
QuikClot is indicated for use in patients who are actively bleeding. We have no public information around the use of QuikClot with paediatric patients. QuikClot works by utilizing kaolin, an inert mineral that activates Factor XII in the blood, which initiates the body's natural clotting cascade. This process accelerates the formation of a clot, helping to control bleeding quickly. There are no risk of emboli, thrombosis, or allergic interactions. Having said that, although we do not have any information of its use in paediatrics, patients clot the same (given normal physiology) regardless of age from birth to death.
QuikClot is indicated for use in the oral cavity, but I must emphasise that the patient should not be left unsupervised when in situ due to the risks associated with choking. This shouldn’t be an issue as a clinician should maintain pressure while in situ. This product also has a radiopaque strip which is X-Ray detectable.
Please let me know if you require any more information.
Best wishes
****
**** ****** HCPC Paramedic, MCPara
Clinical Manager – UK & Ireland
Anaesthesia, Respiratory, Trauma & Emergency Medicine
Clinical & Medical Affairs
P: UK +44 (0)1494 53 27 61 | Ireland +353 0906 46 09 40 | M: +44 7385468226
E: ***********@teleflex.com
Teleflex
TFX Group Ltd, Grosvenor House, Horseshoe Crescent, Old Town Beaconsfield, HP9 1LJ (UK)
Teleflex Medical Europe Ltd, Garycastle, Athlone, Co. Westmeath, (Ireland)
24/9/2025 <***********@teleflex.com> wrote:
Hi *****
I’m glad you did reach out to me. I hope you are well.
She is partly right but QuikClot stopped using zeolite in 2008 and now uses kaolin, a different mineral, as the haemostatic agent in its gauze products. This change was made because the original zeolite formula could cause exothermic reactions and potential tissue damage. The kaolin-based QuikClot devices perform similarly to stop bleeding but without the damaging heat.
This means that there is no chance of exothermic reactions when it is used due to the change of mineral to kaolin back in 2008.
I hope this helps.
Best wishes
****
**** ****** HCPC Paramedic, MCPara
Clinical Manager – UK & Ireland
Anaesthesia, Respiratory, Trauma & Emergency Medicine
Clinical & Medical Affairs
P: UK +44 (0)1494 53 27 61 | Ireland +353 0906 46 09 40 | M: +44 7385468226
E: ***********@teleflex.com
Teleflex
TFX Group Ltd, Grosvenor House, Horseshoe Crescent, Old Town Beaconsfield, HP9 1LJ (UK)
Teleflex Medical Europe Ltd, Garycastle, Athlone, Co. Westmeath, (Ireland)

ATP Clinical incident reporting
The ATP collates and records all kinds of adverse or unexpected incident reports. This information is submitted confidentially with no identifiable patient data; so that the facts and the figures can be quantified to benchmark and audit, to identify risk factor potential and probability.
This may include prolonged bleeding and any additional medical interventions
This is for ATP monitoring and audit which is separate to a CQC notification.
CQC Notification requirements are listed and submitted on their website through your provider portal:
Notifications - Care Quality Commission (https://www.cqc.org.uk/guidance-providers/notifications)

